By: @ericabassotherapy
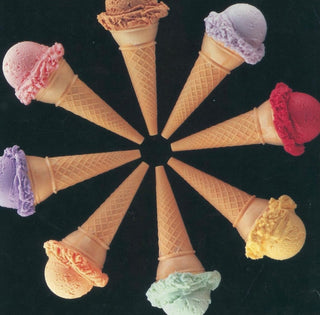
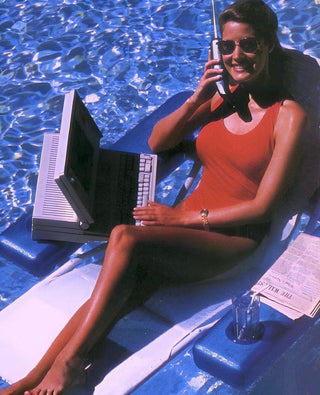
Some people can seemingly have it all: successful career, beautiful family, thriving social life, yet silently fight an internal battle sometimes referred to as “high functioning” depression. I put those words in quotations to highlight the irony of this term and critique why it exists. While high functioning depression is not a formal clinical diagnosis, it is a term that is used to refer to mental distress that seemingly does not impede an individual’s everyday functioning. Society’s standards for functioning ‘well’ typically involves meeting one’s own basic needs, keeping a job, and getting out of bed everyday to perform roles or responsibilities an individual may have. Individuals who experience high functioning depression often fly under the radar due to living up to the standards of functioning set by society. The society we live in values outward achievements, external perceptions, and how much we feel like we are contributing to society’s advancements. It’s necessary that we become better at turning inward, becoming curious and accepting of our internal needs and feelings that require support or healing. These needs may be emotional, finding meaning and/or personal fulfillment.
High functioning depression is similar to the formal mental health diagnosis dysthymia. Dysthymia is a milder form of major depressive disorder with both diagnoses sharing many of the same symptoms, with dysthymia tending to be more long-lasting in an individual's life. Some of the symptoms that dysthymia and major depressive disorder share are:
Sleep issues
Changes in appetite (increase or decrease)
Difficulty concentrating or making decisions
Low energy or fatigue
Feelings of hopelessness
Feeling empty, sad, or down
Low self-esteem
For someone to be diagnosed with major depressive disorder they must meet five of the criteria listed above for a minimum of two weeks, whereas for dysthymia a person must meet two of the criteria for at least two years. It’s often the case that symptoms of dysthymia tend to ebb and flow due to what is occurring in the individual’s life. These shifts in an individual’s behaviors and mood do not usually send off the red flags to others’ that major depressive disorder does. Often an individual learns ways to mask their symptoms so they can still show up for their obligations, but perhaps doing less when symptoms increase or simply doing the bare minimum.
Furthermore, high functioning depression goes overlooked due to held biases about what a depressed person looks like. The stigma surrounding mental health is still prevalent today and is a common barrier to individuals entering treatment. If we see someone ‘successful’ by society’s standards we often fail to exercise curiosity around whether they are mentally well. Individuals with high functioning depression themselves may hold biases around who deserves mental health treatment and who doesn’t. Fear that others may not take them seriously may prevent them from seeking support. It’s often the case that when an individual realizes their outward appearance is not congruent with how they feel inside they feel more shame. As a therapist I often hear the claim, “if only I can be more grateful, hard working, etc. then I will be happy.” Society values the selfless person who overworks and never says no, and individuals may think they just need to do more in order to be happy. The irony is that the more that one over functions, the less likely they are to be connected to their true emotions and needs. Let this be a reminder that just because someone is functioning, does not mean they are well.
As a therapist who works with many successful, well put-together individuals I can tell you the truth is that you cannot always tell when someone is struggling. It’s impossible to truly know what is present in another person’s mind. It can take years before individuals seek appropriate support or therapy because they don't fit the stereotype of a typically “mentally ill” person. Have you ever heard (or if fact stated yourself), “That person doesn’t look like they’re struggling..”? Or maybe you’ve invalidated your own struggles, making comments like, “I shouldn’t complain, others have it worse than me.” Comparative suffering is when we judge, rank, and tally our pain compared to another person’s and it’s harmful to everyone. While it invalidates and minimizes true suffering, it also silences and disconnects us from each other. The presence of certain privileges or protective factors in life certainly can help buffer against the effects of mental health struggles, but it is not a rule for who is and isn’t allowed to suffer with mental health. This isolates individuals in their own pain. When we do this we write off people as not needing help, when most people could benefit from a little extra support, compassion, and knowledge on effective coping tools for mental health.
I vote for a paradigm shift in how we view and treat humans and their mental health. Now more than ever it’s crucial we adopt more critical thinking skills and empathy. We need to start seeing each other for more than what the exterior shows - humans are complex and dynamic.
So what can you do to help?
Practice talking about mental health more often to help normalize the human experience and decrease feelings of isolation. I challenge you to check-in on the friend who seemingly has it all figured out. Or, if you are that friend, check-in with yourself more. How are you really feeling inside? What are you truly needing at this time? Only empathy will connect us.
If you or someone you know is experiencing thoughts of suicide, free-confidential help is available 24/7. Call 1-800-273-8255 or text 988.
References:
https://doi.org/10.1002/jclp.10174
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3130974/
https://journals.sagepub.com/stoken/rbtfl/dDpyhM2zRi.Fg/full
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3698814/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9180102/