By: @dermahealthnutrition
Its profound effect on physical appearance makes alopecia areata (AA) one of the most distressing dermatologic conditions and oftentimes marks a life-changing event for those affected. It is caused by an interplay of several factors: autoimmunity, genetics, and environmental factors. Autoimmunity describes a mistakenly primary attack of the body’s immune system against hair follicles (origin of hair growth). While this attack may result in hair loss, it rarely destroys the hair follicles, implying that your hair can regrow anytime. Oftentimes, AA is associated with other autoimmune diseases such as thyroiditis or inflammatory bowel syndrome. Regarding genetics, one in five affected individuals reports that another family member also has the disease. For example, if a parent has or had AA, a child has a greater risk of developing the disease, which may begin at any age. According to studies, associated environmental factors range from immense stress and COVID-19 infections to cold climate.
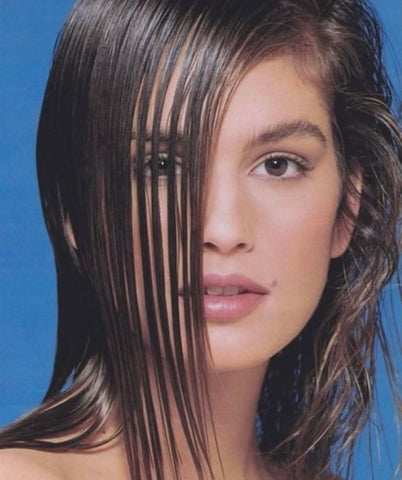
AA can potentially occur in any hair-bearing part of the body, and affect the beard, eyebrows, eyelashes, or pubic hair. Most patients, however, present with round or oval patches of complete hair loss on the scalp. In alopecia totalis, complete baldness is observed. The most pronounced form of AA – alopecia universalis – leaves the entire body hairless, which however is quite rare. Interestingly, AA may also affect the nails, leaving ridges or brittles.
As there are many reasons for hair loss, it is essential to reconfirm the diagnosis with your board-certified dermatologist or functional doctor. A tool called dermatoscope will be used to take a closer look at bald patches.
Signs that you may have alopecia areata:
1. White, fine hairs often remain in bald patches
2. Underlying skin appears to be normal (non-scarring alopecia)
3. With regrowth, the hairs may initially be white, but pigmentation is usually observed within a few months
What you can do
1. Check your blood zinc and vitamin D levels. In case of deficiency take oral supplementation for three months
2. Avoid any unnecessary “hair supplements” without proven deficiency. Consult with a dermatologist or functional doctor and test for any deficiencies or imbalances within the body
3. As the hair loss tends to be unpredictable and regrowth may happen spontaneously (especially if AA has been present for less than a year) avoid too aggressive treatment to avoid potential unnecessary side effects
4. Try not to stress too much as stress may trigger hair loss
5. Have your thyroid tested
6. Consult with a functional medicine doctor for an individualized diet
7. As treatment takes time and especially if hair loss has lowered your self-esteem or causes anxiety openly discuss options including a hairpiece or wig to cover up hair loss for a period of time
8. Shaving the head or beard may help men to cope with patchy hair loss
9. Consult a board-certified dermatologist to talk about further treatment options if necassary (e.g. intralesional corticosteroids, contact immunotherapy, immunomodulators, JAK inhibitors)
For those affected
AA is not contagious
AA usually does not cause any symptoms such as pain or itching
Hair may regrow without treatment (the less hair loss, the more likely)
Clinical studies have recently led to new treatments for widespread forms
The later the onset, the better the chances of regrowth
Some people have cycles of hair loss and regrowth. If this happens, trust in the potential of yet another regrowth episode
References:
Gupta AK, Wang T, Polla Ravi S et al. Systematic review of newer agents for the management of alopecia areata in adults: Janus kinase inhibitors, biologics and phosphodiesterase-4 inhibitors. J Eur Acad Dermatol Venereol 2022, DOI: 10.1111/jdv.18810 Christensen RE, Jafferany M. Association between alopecia areata and COVID-19: A systematic review. JAAD Int 2022; 7: 57-61 Strazzulla LC, Wang EHC, Avila L et al. Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol 2018; 78: 1-12 Korta DZ, Christiano AM, Bergfeld W et al. Alopecia areata is a medical disease. J Am Acad Dermatol 2018; 78: 832-834 Han G. The Changing Landscape of Alopecia Areata: An Introduction. Adv Ther 2017; 34: 1584-1585 Putterman E, Castelo-Soccio L. Seasonal patterns in alopecia areata, totalis, and universalis. J Am Acad Dermatol 2018; 79: 974-975