By: @drmelissa_co
Insulin, like all hormones, plays an integral role in the way our bodies work. Energy levels, mood, how fast (or slow) one’s metabolism is, if and where weight is stored, the ability to focus and overall brain health, the female menstrual cycle, libido, fertility, skin quality, cardiovascular wellness...all of these functions, among many others, rely on how insulin is released and how our bodies respond to it.
Insulin resistance is a condition in which the body does not properly respond to this hormone, which eventually wreaks havoc on blood sugar levels. This is a condition I see very regularly in practice, and one that often flies under the radar for years. Insulin resistance left untreated over time can increase the risk of various chronic diseases including diabetes and cardiovascular disease. It is very common with increased weight but can be present in people of normal weight, and it is a condition that often plays a role in Polycystic Ovarian Syndrome (PCOS). Everyone is at risk of insulin resistance, and it would be beneficial for all of us to learn about this condition and how to prevent it.
A master at regulating blood sugar, insulin is a central hormone of metabolism. After eating, the digestive tract breaks down food into simple molecules that are absorbed into the bloodstream where they travel to cells for use. Once we eat, the pancreas detects glucose (or sugar, the building blocks of all carbohydrates) in the bloodstream and begins to release insulin. Insulin is what helps the cells absorb this glucose—which is a great energy source that keeps your cells working.
I like to use this analogy: as glucose floats through the bloodstream, insulin is released. This insulin begins to knock on the doors of your cells, letting them know glucose is here, ready to be absorbed and used as energy. In someone who has a healthy response to insulin (also known as insulin sensitive—the opposite of resistant), the doors of your cells most always open in response to this knock from insulin. The cells then absorb glucose efficiently and use it as cellular fuel to do all the jobs they need to do. Insulin also allows glucose to be effectively stored in the liver for energy later, as needed, when we are fasted. This is the ideal scenario. In someone who is insulin resistant, this knock is answered less frequently by the cells, leaving sugar unused in the bloodstream. In someone with type II diabetes, the cells hardly ever answer this knock, if at all, and sometimes the body stops releasing insulin altogether. Type I diabetes on the other hand, involves no production of insulin; there is no knock on the door in the first place. In both types of diabetes and in insulin resistance, glucose is left floating around in the blood stream which poses many risks long-term.
Short term, hyperglycemia, or too much sugar in the blood stream causes issues with mood, energy, menstrual cycles, sexual health, weight and metabolism, and more. Over time, hyperglycaemia causes fatty liver disease and damages blood vessels which supply our vital organs; there is an increased risk in heart disease, stroke, issues with vision, nerve concerns, kidney disease, among other concerns. In short, keeping blood sugar well balanced and insulin sensitivity strong is a very worthwhile pursuit.
Insulin resistance arises over time as a result of poor or irregular eating habits, increased sugar, flour, alcohol or other processed carbohydrate consumption, lack of protein, healthy fats, fruits and vegetables, inactivity, and genetics. Unfortunately, a lack of education around nutrition and lifestyle medicine as well as lack of access to whole foods also makes this condition more prevalent.
So, how can you prevent and possibly mitigate insulin resistance? It is all about keeping blood sugar as steady as possible, and helping your body stay sensitive to insulin. Here are my top tips:
1. Eat breakfast: eating breakfast within 90 minutes of waking can stabilize blood sugar early in the day and mitigate sugar cravings later, BUT:
2. make sure breakfast contains protein and a healthy fat: some great options include eggs and avocado with a side of berries, a mixed vegetable, omelet made with olive oil, organic yogurt with berries, raw nuts and seeds. These are blood sugar stabilizing options.
3. Consider the order in which you eat your food: see my recent article for more information https://www.sportyandrich.com/blogs/wellness/controlling-blood-sugar-with-food-sequencing
4. Consider low glycemic index foods: a quick web search will yield a list of foods that are low glycemic, or do not spike blood sugar easily. Eat these more regularly or in place of higher glycemic foods.
5. Include apple cider vinegar in your diet: see my recent article for details on this amazing ingredient that helps to regulate blood sugar spikes— https://www.sportyandrich.com/blogs/wellness/apple-cider-vinegar-folk-remedy-proven-by-science
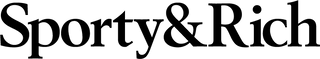
6. Exercise: at least 30 minutes of moderate exercise per day is absolutely necessary to keep your cells sensitive to insulin. Moderate exercise refers to movement that is rigorous enough that you could hold a conversation while doing it, but you would not be able to sing. This includes brisk walking, weight training, certain forms of Pilates and yoga.
7. Move after a large meal: resist the urge to crash on the couch and get moving after a large meal or one that contains sugar or carbohydrates. Taking a 15 minute brisk walk shortly after a large meal can blunt the blood sugar spike and improve your muscle’s ability to remove and utilize glucose from the bloodstream.
8. Supplement: certain supplements are incredibly powerful and helpful at regulating insulin and blood glucose levels. Ingredients like inositol and berberine are two I commonly use in my practice. These should only be considered if you have had regular screening blood work, and must be dosed appropriately. Speak to your naturopathic or functional medicine doctor before supplementing.
While supplementation should only be considered when labs are abnormal, my other recommendations can be explored as great preventative strategies to support blood sugar and insulin levels. As always, individualized recommendations are always best. Speak to your primary care doctor for regular visits and screening tests. Having your fasting glucose, fasting insulin and having your HOMA-IR calculation done by your doctor will help you better understand how insulin sensitive or resistant you are.
Resources: